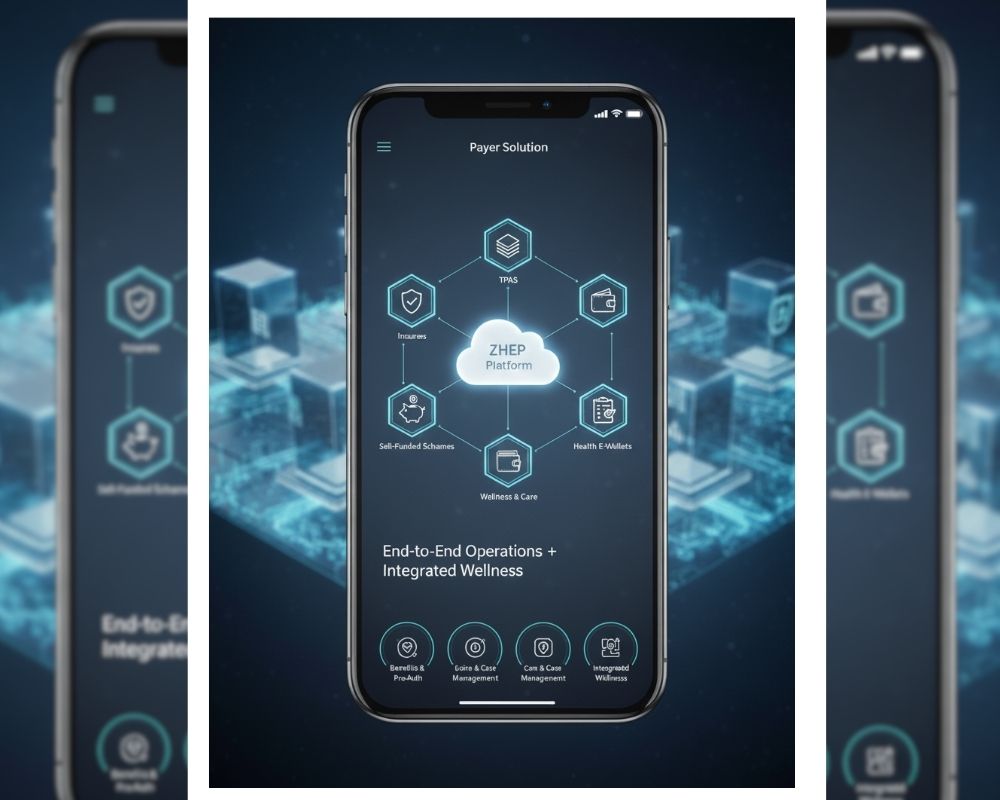
Payer Solution
Built for insurers, TPAs, self-funded schemes, and health e-wallets. Operate benefits, pre-auth, care/case, claims & finance—and integrate wellness via ZHEP.
Core Modules
- Product & benefits · Enrollment · Provider & tariffs · Authorizations · Care/Case mgmt · Claims/adjudication · Payouts/reconciliation · Analytics
Interoperability
- Modern APIs & FHIR so HIS/EMR, labs, and claims talk to each other.
Outcomes
- Higher activation and redemption; clearer reporting for executives.
> AI, safely: Pre-auth triage, claims anomaly signals, next-step prompts—human-reviewed with audit trails.